
Naringenin und Covid-19
Das Flavanon Naringenin hat positive Wirkungen auf die Lunge und wurde schon als Mittel gegen Covid-19 getestet.
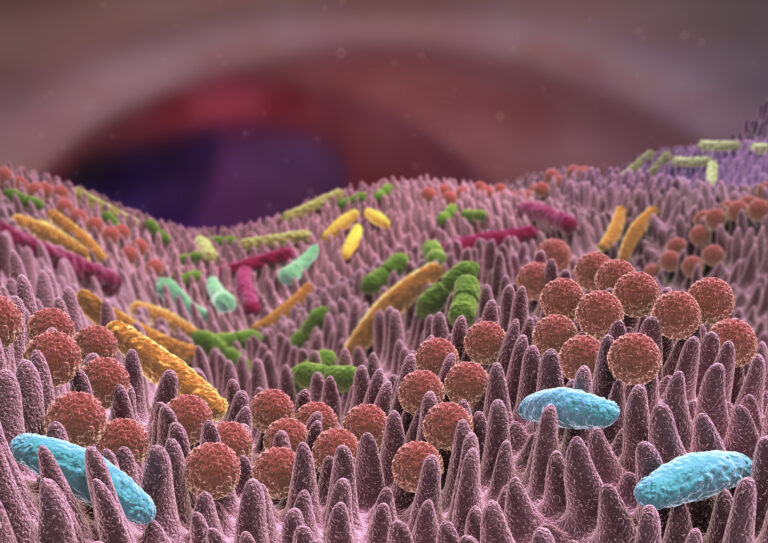
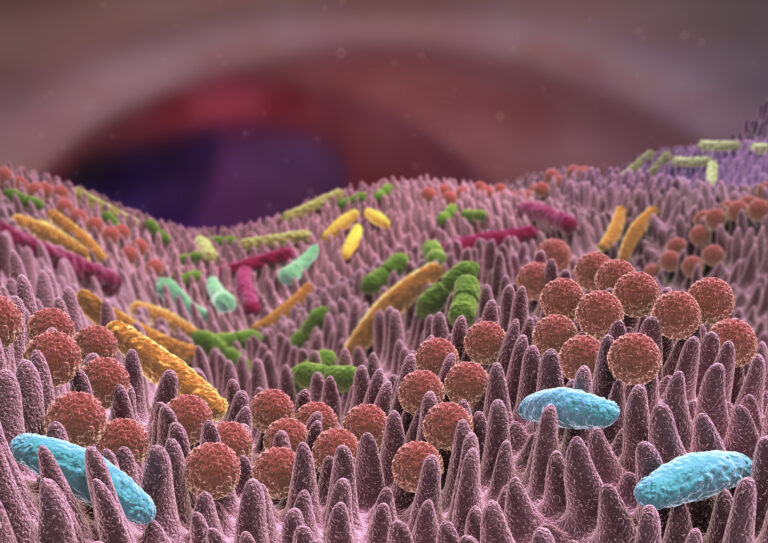
The microbiome refers to the totality of the trillions of bacteria, fungi and viruses that colonize our intestines and have a previously underestimated influence on our health [1,2]. They are small but extremely numerously! On a square centimeter in the intestine there are more living beings than humans on Earth. It is the most densely populated known habitat. After all, the totality of the microbiome in an adult person weighs between 1-2 kilograms, which we carry around with us every day. One can well imagine that the community exerts a considerable influence on health [3],[4]. A hype has grown up around the microbiome in recent years and research is progressing rapidly. If you enter the search term "good microbiome" in the most frequented meta-databases for scientific publications – PubMed –you get 28,932 hits (as of March 2021), whereby the high publication activity started in 2015. It will reach its maximum in 2019/2020 with around 7000 publications per year. From a therapeutic point of view, the microbiome represents a less-used way to maintain health. The microbiome works best when it has a high diversity of the bacterial community to cope with the wide range of tasks [5].
The tasks of the bacteria are to break down undigested food in the large intestine, to form a barrier for pathogens that could enter the body via the intestine, to produce certain vitamins and hormones, to promote the development and maturation of the immune system, to support the cells of the intestinal mucosa in their function and to keep us healthy. The huge number of bacteria therefore lives in good symbiosis with their host. The ailments that can be associated with dysbiosis, on the other hand, are very diverse. Meanwhile, 90 % ! of all diseases associated with the microbiome or intestinal health. There is practically no organ left that is not affected by the microbiome [6]. For far too long, the influence of the mass of bacteria on health has been underestimated. Even the influence on our psyche takes place in a way that was thought unimaginable until recently [7]. Microbial changes due to obesity, for example, are sufficient for this [8]. The fact is that the microbiome is involved in controlling complex processes in the body. Both physical and mental health are related, among other things, to the composition of the bacteria. The well-being of these tiny creatures is inextricably linked to our own happiness.
The microbes produce various vitamins and neurotransmitters for us, which have a direct influence on health. They also influenc indirectly our health by a main product of bacterial metabolism, the short-chain fatty acids (Short Chain Fatty Acids – SCFA). These leave the intestine and have a systemic effect [9]. They are absorbed by almost all tissues, including the brain. Around one third of the demand is covered by the microbiome. Short-chain fatty acids supply the cells of the intestinal mucosa with energy, they are involved in the regulation of appetite and energy metabolism. Various animal studies and a small number of human studies show that increased microbial production of short-chain fatty acids can help prevent and treat metabolic diseases such as type 2 diabetes mellitus and obesity [10].
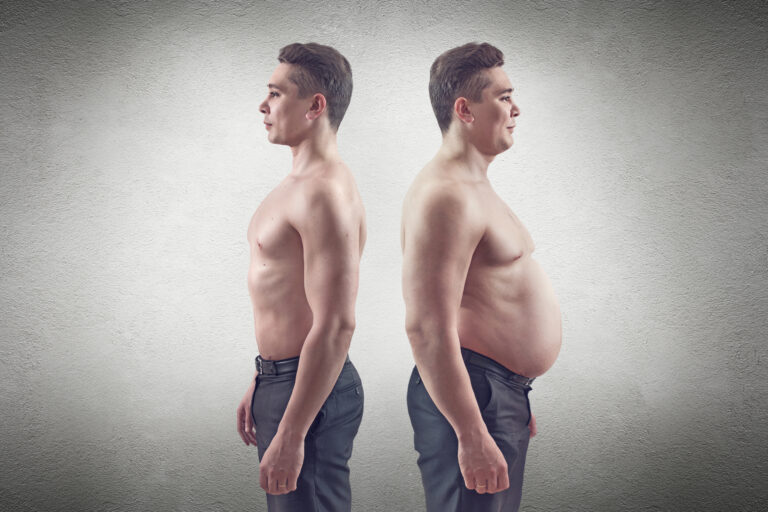
Because microbial metabolism produces metabolites that exert far-reaching, systemic effects, the microbiome is already referred to as having its own "metabolic organ" with a potential comparable to that of the liver [11]. The microbiome influences sugar and fat metabolism through metabolites and these metabolites change when you are overweight [12]. Despite all individuality, certain changes correlate with certain health conditions. An unfavorably altered microbiome, for example, has an influence on the immune defense [13,14], cardiovascularsystem[15]. Intestinal diseases [16], vitamin production [17], skin [18], diabetes [19], cancer [20], the psyche [7] or obesity with the associated sequelae [21] [22] [23]. Fecal transplants of twins, in which one is overweight and the other has a normal weight, have been used in germ-free mice. The animals that were given the stool of the overweight twin gained weight, while the other mice remained slim, although they ate little differently [24]. Such and similar exciting experiments on fecal transplants [25] underline the potential of the microbiome.

Anything that the small intestine does not process enters the large intestine. There, the bacteria decompose various food components that humans cannot digest or have not digested. The possibilities of the bacteria to do this are many times higher if one compares the genetic potential of the bacteria, which together have almost 4 million genes, to humans, which come to about 20,000 genes [26], [27]. From an evolutionary point of view, this was probably a way to open up more and new food when the microbiome still provides humans with energy from actually indigestible substances. In today's afluent society, however, we are more than enough supplied with calories. Japanese, for example, have an intestinal bacterium capable of digesting seaweed, such as whose stuff is used for sushi. Europeans and Americans do not possess this bacterium.
On the one hand, the microbiome represents a very flexible structure – the microbiome can change within hours. Bacteria have a generation time of 20 min and would show exponential growth under ideal conditions. So those who find the best feeding conditions also multiply the fastest: the microbiome changes practically after every meal. Furthermore, rapid changes to changing environmental conditions can be observed. In long-distance runners, a particularly large number of bacteria have been found in the intestine after a marathon that break down lactic acid. This is the substance that accumulates in the muscles during long exertion and ultimately weakens them.
These are rapid changes to external environmental conditions. As long as you eat a variety of things and alternately different species are regulated up and down, that's no problem. But if a person eats too many ready meals, meat or sugar, this can put the bacterial community in trouble in the long run. Then the diversity decreases and harmful bacteria get the upper hand, which produce e.B. toxins or trigger inflammation. Depending on the intensity of the impact, a permanent imbalance takes months to years to adjust permanently. It takes just as long to regenerate. With the yo-yo effect, for example, it takes up to 15 weeks after a diet for the dysbiotic, overweight microbiome to normalize (see yo-yo effect). After some antibiotic treatments, it also takes months for the intestine to regenerate. There can also come longer to an irritable bowel syndrome and in some cases the intestine even permanently no longer works as before. Then some species simply disappeared. It depends on the variety and this can only be achieved through a varied, plant-based diet.
[1] Álvarez, J. et al. Gut Microbes and Health. Gastroenterol Hepatol. (2021), 27: 0210-5705(21)00058-3.
[2] Dave M. et al. The human gut microbiome: current knowledge, challenges, and future directions. Transl Res. (2012),160(4): 246–57.
[3] Carding, S. et al. Dysbiosis of the gut microbiota in disease. Microb. Ecol. Health Dis. (2015), 26: 26191.
[4] Guarner, F. and Malagelada, J.R. Gut flora in health and disease. Lancet (2003), 361: 512–519.
[5] Ley R.E. et al. Ecological and evolutionary forces shaping microbial diversity in the human intestine. Cell (2006),124(4): 837–48.
[6] Ahlawat, S. et al. Gut-organ axis: a microbial outreach and networking. Lett Appl Microbiol. (2020), doi: 10.1111/lam.13333.
[7] Sarkar, A. et al. Psychobiotics and the manipulation of bacteria-gut-brain signals. Trends Neurosci (2016), 39: 763–781.
[8]Torres-Fuentes, C. et al. The microbiota-gut-brain axis in obesity. Lancet Gastroenterol Hepatol. (2017), 2(10): 747-756.
[9] Mohamed, S.D. and Fischbach, M.A. Small Molecules from the Human Microbiota. Science (2015), 349 (6246): 1254766
[10] Campos-Perez, W. and Martinez-Lopez, E. Effects of short chain fatty acids on metabolic and inflammatory processes in human health. Biochim Biophys Acta Mol Cell Biol Lipids (2021),1866(5):158900.
[11] Guinane, C.M. and Cotter, P.D. Role of the gut microbiota in health and chronic gastrointestinal disease: understanding a hidden metabolic organ. Therap Adv Gastroenterol. (2013), 6(4): 295–308.
[12] Aoun A. et al. The Influence of the Gut Microbiome on Obesity in Adults and the Role of Probiotics, Prebiotics, and Synbiotics for Weight Loss. Prev Nutr Food Sci. (2020), 25(2): 113–123.
[13] Hooper, L.V. et al. Interactions between the microbiota and the immune system. Science (2012), 33 6(6086):12 68–73.
[14] Jarchum, I. and Pamer, E.G. Regulation of innate and adaptive immunity by the commensal microbiota. Curr Opin Immunol. (2011), 23(3): 353–60.
[15] Witkowski, M. et al. Gut Microbiota and Cardiovascular Disease. Circ Res. (2020),127(4): 553-570.
[16] Van den Houte, K. et al. Recent advances in diagnosis and management of irritable bowel syndrome. Curr Opin Psychiatry. (2020), 33(5): 460-466.
[17] Ramakrishna, B.S. et al. Role of the gut microbiota in human nutrition and metabolism. J Gastroenterol Hepatol. (2013), 28: 9–17.
[18] Sikora, M. et al. Gut Microbiome in Psoriasis: An Updated Review. Pathogens. (2020), 9(6): 463.
[19] Katya Frazier, K. and Leone, V.A. Microbiota Can’t Keep Time in Type 2 Diabetes Cell Host Microbe. (2020), 28(2): 157-159.
[20] Dikeocha, I.J. et al. Role of probiotics in patients with colorectal cancer: a systematic review protocol of randomised controlled trial studies. BMJ Open. (2020), 10(8): e038128.
[21] Ley, R. E. Obesity and the human microbiome. Curr. Opin. Gastroenterol. (2010), 26: 5–11.
[22] Aoun A. et al. The Influence of the Gut Microbiome on Obesity in Adults and the Role of Probiotics, Prebiotics, and Synbiotics for Weight Loss. Prev Nutr Food Sci. (2020), 25(2): 113–123.
[23] Wicinski, M. et al. Probiotics for the Treatment of Overweight and Obesity in Humans—A Review of Clinical Trials. Microorganisms (2020), 8: 1148.
[24] Ridaura, V.K., et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science (2013), 341: 1241214.
[25] Vrieze, A. et al. Transfer of Intestinal Microbiota from Lean Donors Increases Insulin Sensitivity in Individuals with Metabolic Syndrome. Gastroenterology (2012), 143: 913–916.
[26] Yadav M. et al. A review of metabolic potential of human gut microbiome in human nutrition. Arch Microbiol (2018), 200(2): 203-217.
[27] Linares, D. M. et al. Beneficial microbes: the pharmacy in the gut. Bioengineered (2016), 7: 11–20.

Das Flavanon Naringenin hat positive Wirkungen auf die Lunge und wurde schon als Mittel gegen Covid-19 getestet.
Das Mikrobiom mischt bei Demenz, Autismus und Herzinfarkten mit. Billionen Bewohner des Verdauungstrakts werden künftig zu Therapeuten.

Die Lunge profitiert von antioxidativen und antiinflammatorischen Pflanzenstoffen.

Das Flavanon Naringenin hat positive Wirkungen auf die Lunge und wurde schon als Mittel gegen Covid-19 getestet.
Das Mikrobiom mischt bei Demenz, Autismus und Herzinfarkten mit. Billionen Bewohner des Verdauungstrakts werden künftig zu Therapeuten.

Die Lunge profitiert von antioxidativen und antiinflammatorischen Pflanzenstoffen.
80% aller Hungerkuren scheitern. Um der Statistik des Scheitern entgegenzuwirken, gibt es jetzt etwas gegen den Jo-Jo-Effekt aber auch ein paar grundsätzliche Dinge sollten beachtet werden.
| Cookie | Dauer | Beschreibung |
|---|---|---|
| cookielawinfo-checbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |