
Naringenin und Covid-19
Das Flavanon Naringenin hat positive Wirkungen auf die Lunge und wurde schon als Mittel gegen Covid-19 getestet.
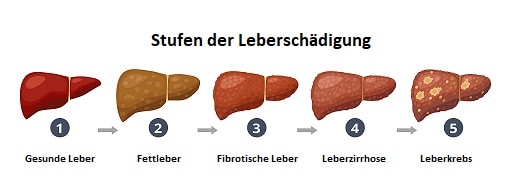
Liver diseases are usually symptom-free (except for non-specific symptoms such as fatigue, reduced performance, lack of concentration) and are often only discovered by chance diagnosis. Starting from the healthy liver, fatty liver disease develops due to the pathological accumulation of lipid droplets in the hepatocytes. The fatty liver is curable in its course. Only when the liver tissue changes, irreversible damage threatens. Non-alcoholic fatty liver disease (NAFLD) is a multifactorial liver disease whose incidence is increasing worldwide. Cardiovascular disease and type II diabetes are closely linked to NAFLD [1]. NAFLD-related liver failure has become the second leading cause of liver transplants in Western countries [2]. Lifestyle changes, i.e. the implementation of a change in diet and more exercise is a mainstay in the treatment. Developments in diets and dietary supplements to prevent NAFLD represent a major need [3]. Microbiome-active flavanones represent a new, promising alternative, as they relieve the liver via several pathways.
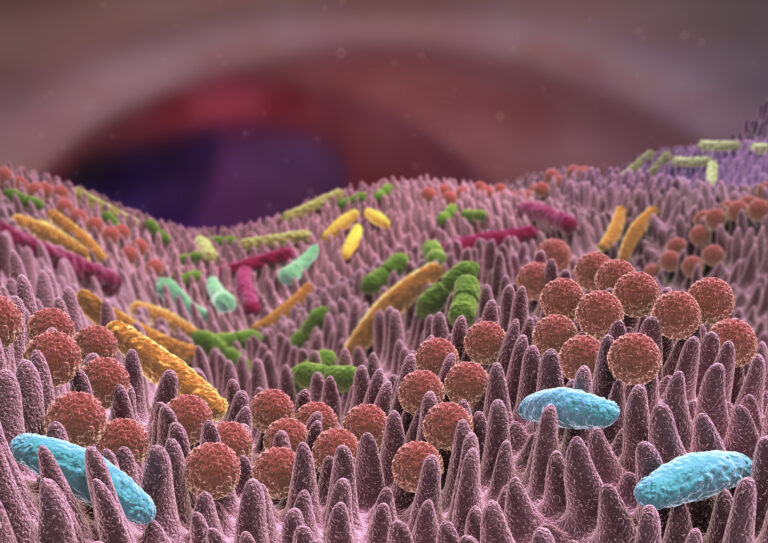
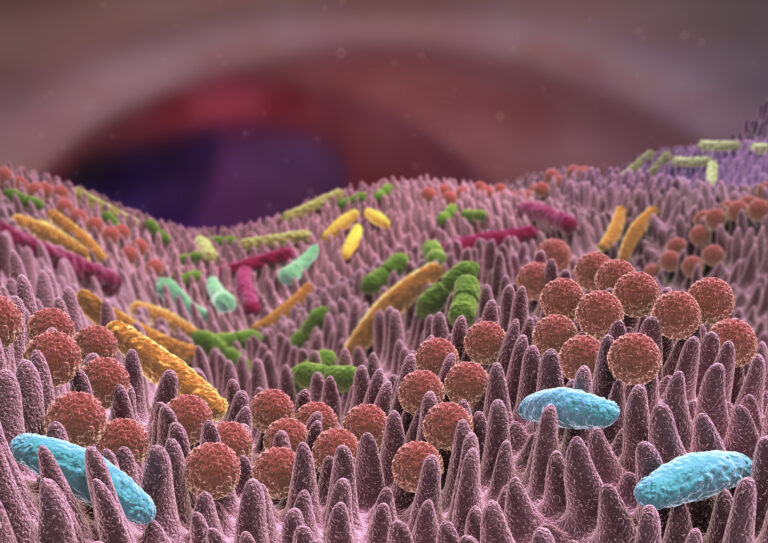
The gut bacteria affect fat metabolism and lipid levels in the blood and tissues, both in mice and humans [4], [5]. Fecal transplants from mice fed high fat levels led to weight gain and metabolic syndrome in germ-free recipient mice [6]. Interestingly, germ-free mice without gut bacteria are resistant to diet-related obesity, steatosis, and insulin resistance [7]. Gut bacteria represent a new therapeutic target against NAFLD [8]. In 2020, Mu et al. have shown that naringenin exerts its effect against fatty liver via the microbiome [9]. The scientists consider the substance to be as effective as drugs that regulate fat or sugar metabolism. The role of naringin's prebiotically altered microbiota in lowering cholesterol has also been studied by Wang et al. Naringin significantly helped against atherosclerosis and improved cholesterol levels by 28%. Naringin increased the production of bile acid and neutral sterols by up to 4.3 times. They were able to show that naringin mainly exerts its effect via the microbiome-liver-cholesterol axis [10]. The cholesterol-lowering effect of the grapefruit substance and its positive effect on diabetes symptoms had already been suggested by previous studies. The citrusflavonoid activates two proteins in its metabolized form and blocks a third in liver metabolism. This leads to an increased breakdown of fatty acids and ultimately lowers the proportion of "bad" LDL cholesterol. Naringenin stimulates metabolic processes in the liver that are comparable to a fasting cure. The liver usually prepares fatty acids for long-term storage. Through naringenin, however, she breaks down these fatty acids, as during a strict diet [11],[12], which gives him great therapeutic potential for the treatment ofNAFLD. Since the intestinal bacteria play a central role in the development of NAFLD, naringin has a positive effect on liver values by modulating the composition of intestinal bacteria. Naringin reduces both weight gain and fat accumulation in the liver. The changes in the bacterial community are characterized by the growth of beneficial species and reduction of less pathogenic species. Individual species have even been identified (genus) that are negatively correlated with high blood lipid levels: Allobaculum, Alloprevotella, Butyricicoccus, Lachnospiraceae_NK4A136_group, Parasutterella and uncultured_bacterium_f_Muribaculaceae. And in return, species that have a positive effect on blood lipid levels: Campylobacter, Coriobacteriaceae, Faecalibaculum and Fusobacterium [9].
.

The liver is the central point for fat and sugar metabolism. Naringenin influences hepatic fat metabolism via PPAR receptors (peroxisomeproliferator-activatedreceptors) [13]. These are intracellular receptors that are activated via a small molecule ligand and then regulate the expression of a variety of genes. So far, three PPAR subtypes (α, β, γ) have been identified in the human organism. These differ not only in their local location, but above all in terms of their gene expression pattern and the biological function of the genes that is influenced by them [14]. PPARα is highly expressed in the liver, kidneys, intestines and heart. The activation of PPARα primarily has effects on blood lipid levels: Among other things, it causes a reduction in circulating triglycerides, an increase in the intake of free fatty acids, an increase in fatty acid oxidation and an increase in HDL while simultaneously reducing LDL concentration. In addition, the activation of PPARα has anti-inflammatory effects. PPARβ is detectable in almost all tissues of the human organism. The β receptor primarily regulates the expression of genes with an effect on fat metabolism. In experiments on obese animals, the activation of PPARβ resulted in an improvement in various metabolic parameters as well as a reduction in body weight [15]. PPARγ is ubiquitously expressed. The activation of PPARγ causes in particular an improvement in glucose metabolism and insulin sensitivity. Furthermore, the activation of the PPARγreceptor increases the absorption of free fatty acids and acts on the differentiation of adipocytes and macrophages.
Goldwasser et al. have found that naringenin is the only LXR inhibitor of natural origin [16]. Liver X receptors (LXRs) are molecule-activatable transcription factors involved in cholesterol metabolism, inflammatory mechanisms and lipogenesis. LXRs are mostly found on the liver, kidneys and adipose tissue. The activation of LXRα (liver) results in high triglyceride production. The citrus flavanones have a lowering effect on blood lipid levels due to inhibition. In addition, they reduce concomitant inflammatory reactions in various tissues including the liver, adipose tissues, kidneys and aorta. The anti-atherosclerotic effect is also achieved by a direct effect on the blood vessels [17]. Liver impairment can also affect the heart via atherosclerosis [18] and is therefore potentially life-threatening. It is therefore an extremely far-reaching health function of microbiome-active flavanones to relieve and protect the liver.
Liver damage is associated with systemic, oxidative stress leading to lipidperoxidation, tissue damage, fibrosis, or even cell death. Due to the lack of hepatoprotective drugs, plant-based substances represent a significant alternative. Naringenin in particular has come into focus due to its antioxidant, anti-inflammatory and cell-protecting activity. In traditional Chinese medicine, Aurantii Fructus Immaturus and Aurantii Fructus are often used against liver disease. Wu et al. have found in 2020 that it is the flavanones in the plant that act in the liver through several mechanisms[19]. These include the antioxidant properties, the cell-protecting effect, anti-fibrotic properties, anti-inflammatory and anti-cancer mechanisms. This is also confirmed by Shirani et al., who have summarized the effects of naringenin for liver protection in a review[20].
Diet is a big adjusting screw in lowering blood lipid levels. This does not include giving up cholesterol-containing foods. If too little cholesterol is ingested with food, the liver simply produces more. You can replace saturated fats with unsaturated dietary fats and eat low-carb foods. From the carbohydrates in the diet, the liver builds a fatty acid called palmitic acid, which causes cholesterol levels to rise much more than the fat in food. The path via the microbiome and targeted microbiome-active food supplementation represents an additional, promising adjustment screw.

Das Flavanon Naringenin hat positive Wirkungen auf die Lunge und wurde schon als Mittel gegen Covid-19 getestet.
Das Mikrobiom mischt bei Demenz, Autismus und Herzinfarkten mit. Billionen Bewohner des Verdauungstrakts werden künftig zu Therapeuten.

Die Lunge profitiert von antioxidativen und antiinflammatorischen Pflanzenstoffen.

Das Flavanon Naringenin hat positive Wirkungen auf die Lunge und wurde schon als Mittel gegen Covid-19 getestet.
Das Mikrobiom mischt bei Demenz, Autismus und Herzinfarkten mit. Billionen Bewohner des Verdauungstrakts werden künftig zu Therapeuten.

Die Lunge profitiert von antioxidativen und antiinflammatorischen Pflanzenstoffen.
80% aller Hungerkuren scheitern. Um der Statistik des Scheitern entgegenzuwirken, gibt es jetzt etwas gegen den Jo-Jo-Effekt aber auch ein paar grundsätzliche Dinge sollten beachtet werden.
| Cookie | Dauer | Beschreibung |
|---|---|---|
| cookielawinfo-checbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |